[TDMC]-What You Need to Know about Atopic Eczema and Food Allergy

[TDMC] Live Cell Therapy: Past, Present, and Future
8 December 2022
[TDMC]-What You Need to Know about Contact Dermatitis
21 December 2022
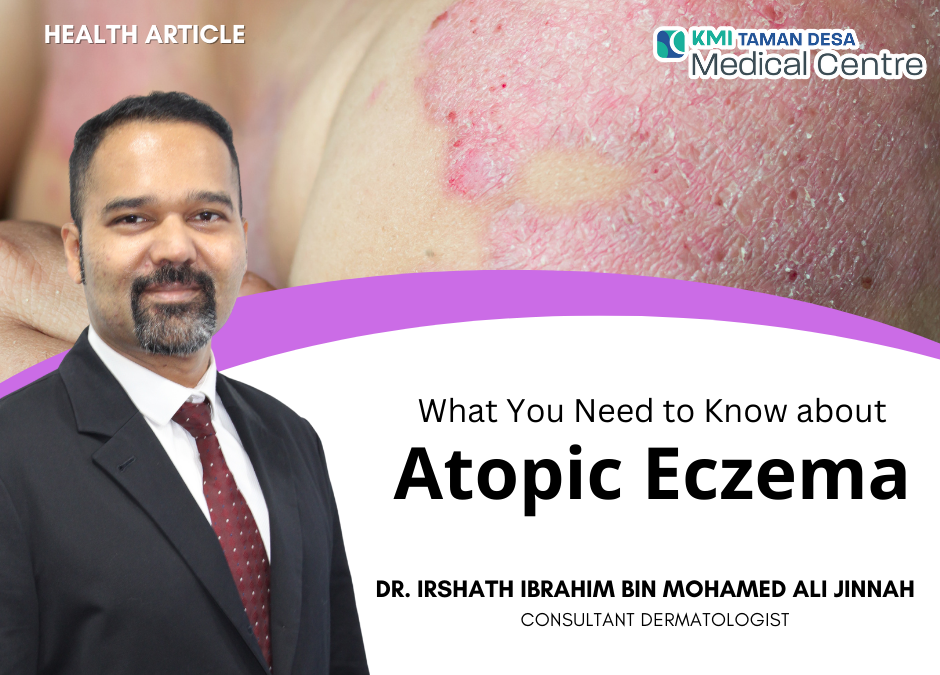
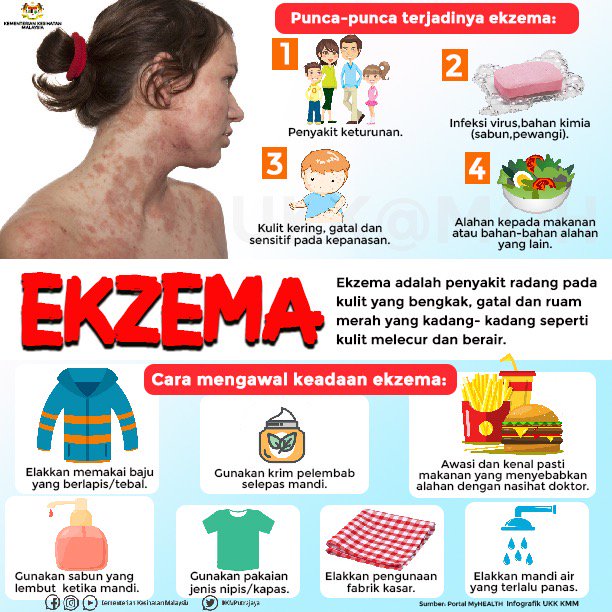
1.What is Atopic Eczema?
Atopic eczema (AE) is an inflammation of the skin that results in itch, rash and dryness. It is also known as the ‘itch that rashes’ because when the itching starts, rash will soon appear due to scratching or rubbing.

2.What is Atopy?
The word atopy originates from atopos in Greek meaning ‘out of place’.
3.Is atopic eczema the same as atopic dermatitis?
Yes. AE is also known as atopic dermatitis(AD).
The term eczema is derived from ancient Greek that means boiling out or boiling over.
Ancient Chinese medicine referred eczema as jin yin chuang (wet spreading sore), shi zhen (damp eruption) or feng shi chuang (wind damp sore).
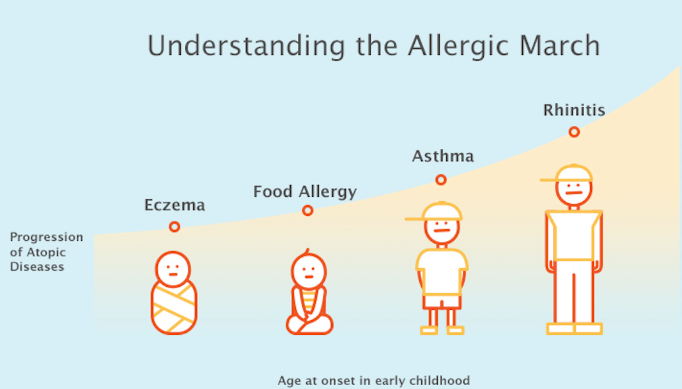
4.What is atopic march?
Comprises of AD and other associated conditions such as food allergies, asthma and allergies affecting the nose and eyes (rhinoconjunctivitis).



Photo Source: Freepik.com
5.How common is AE?
Approximately 230 million people worldwide have AE.
6.Is cradle cap the same as AE?
Cradle cap or the medical term ‘infantile seborrhoeic dermatitis’ is a form of eczema that affects babies < age of 3 months but usually resolves by the age of 6 months unlike AE which can persist longer.

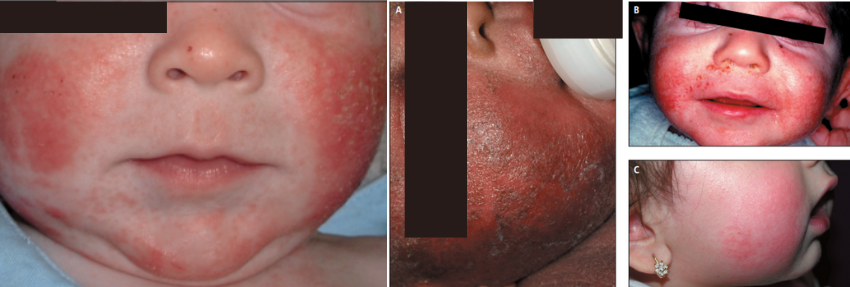
7.Where does the rash of AE usually appear?
It can appear anywhere on the patient’s skin surface but the distribution varies according to age.
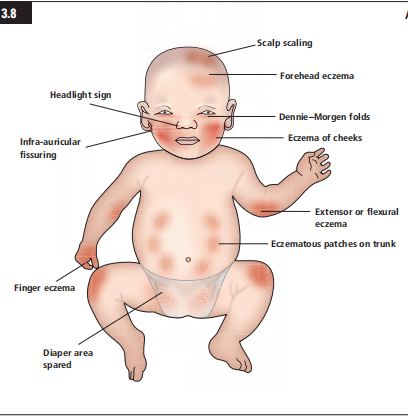
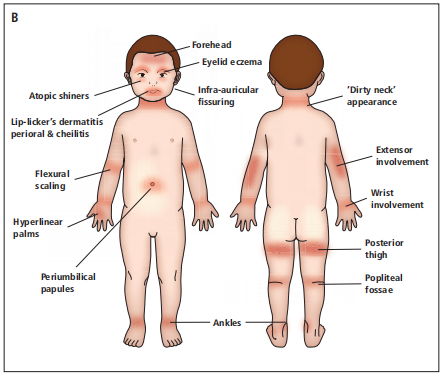
Source: Rudikoff, D., Cohen, S., & Scheinfeld, N. (Eds.). (2014). Atopic Dermatitis and Eczematous Disorders (1st ed.). CRC Press
8.What is the prevalence of atopic eczema in children and adults?
About 10-30% in children and 2-10% in adults.
9.What age does AE usually develop?
- 45% develop before the age of 6 months old.
- 60% develop by 1 year of age.
- 85% develop before the age of 5 years old.
10.Can I develop AE at an older age?
Yes. This is known as late onset AE which develops after puberty or senile onset AE which develops after the age of 60 years old.
11.Can atopic eczema (AE) run in the family?
Yes. If AE is present in either parent, it poses a strong risk factor for the children to develop AE as well.
12.What are the risks if a genetic mutation is the cause of AE?
20-50% of European and Asian children with moderate to severe AE have a genetic mutation. This puts them at risk of developing AE at an early age, more severe disease, increase risk of contact dermatitis, skin infections, food allergy. AE can persist into adulthood.
13.Why are genes important in preventing AE?
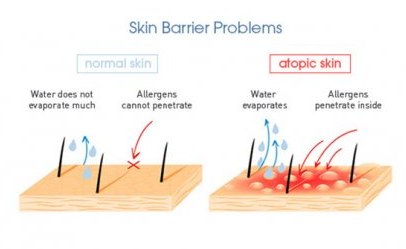
Certain genes eg FLG, FLG2 are important in preserving our skins natural protective barrier. A breakdown in the skin’s protective barrier allows the entry of allergens, irritants or bacteria which will initiate skin inflammation leading to AE.
14.If a patient has a family history of AE, is it necessary to do a genetic screening?
AE can be diagnosed clinically from examination. A genetic screening is not mandatory. If there is doubt in diagnosis, a skin biopsy will be advised for the patient.
15.What tests can a patient with AE undergo?
When indicated, tests are mainly to check for allergies towards food, environmental allergens, contact dermatitis.
16.Can AE completely resolve?
About 60% of infants and young children are fortunate to go into remission by the age of 12 years old. However, AE can persist into adolescence and adulthood.
17.What sort of bathing methods should a patient with AE adopt?
- Bathe in lukewarm water 1-2x/day with gentle cleanser for < 10 minutes.
- Air dry or gently pat wet areas with soft cotton towel but avoid rubbing.
- Apply moisturizer after a bath.
18.If the skin’s protective barrier is compromised, is the affected person more prone to infections, irritants or allergens?
Yes. Once the skin’s barrier is compromised, bacteria, irritants, allergens will be able to enter the skin and cause inflammation.
19.What are examples of allergens that cause or aggravate AE?
Dust, mite, pollen, animal dander, fungi.
20.What are examples of irritants that can cause or aggravate AE?
Nylon, wool, sweat, soap, shampoo, detergent, disinfectants, traditional oils or creams, non evidence based medicines.
21.Is a patient with chronic AE susceptible to heart disease?
Yes. The overall inflammation of chronic AE has a modest association with heart disease.
22.Can AE affect the mental and emotional state of a patient?
Yes. It can be mentally detrimental to children especially leading to psychological and psycho-social dysfunction.
23.Is the prevalence of AE higher in active and passive smokers?
Yes.
24.Will AE worsen during pregnancy?
Roughly >50% of pre-existing AE tends to worsen during pregnancy due to the hormonal changes associated in pregnancy that directly affects the type of immunity response.
25.Can breast milk reduce the risk of developing AE?
Yes. Exclusive breast feeding for the first 6 months or formula containing hydrolyzed milk may reduce the risk of AE.
26.Is cow’s milk helpful in reducing the risk of AE?
Most of the infant formulas are derived from cow’s milk that has been altered to resemble breast milk hence providing the necessary nutrients a growing infant requires. Most babies do well on cow’s milk however the protein from cow’s milk may cause cow milk protein allergy (CMPA) which can potentially aggravate AE.
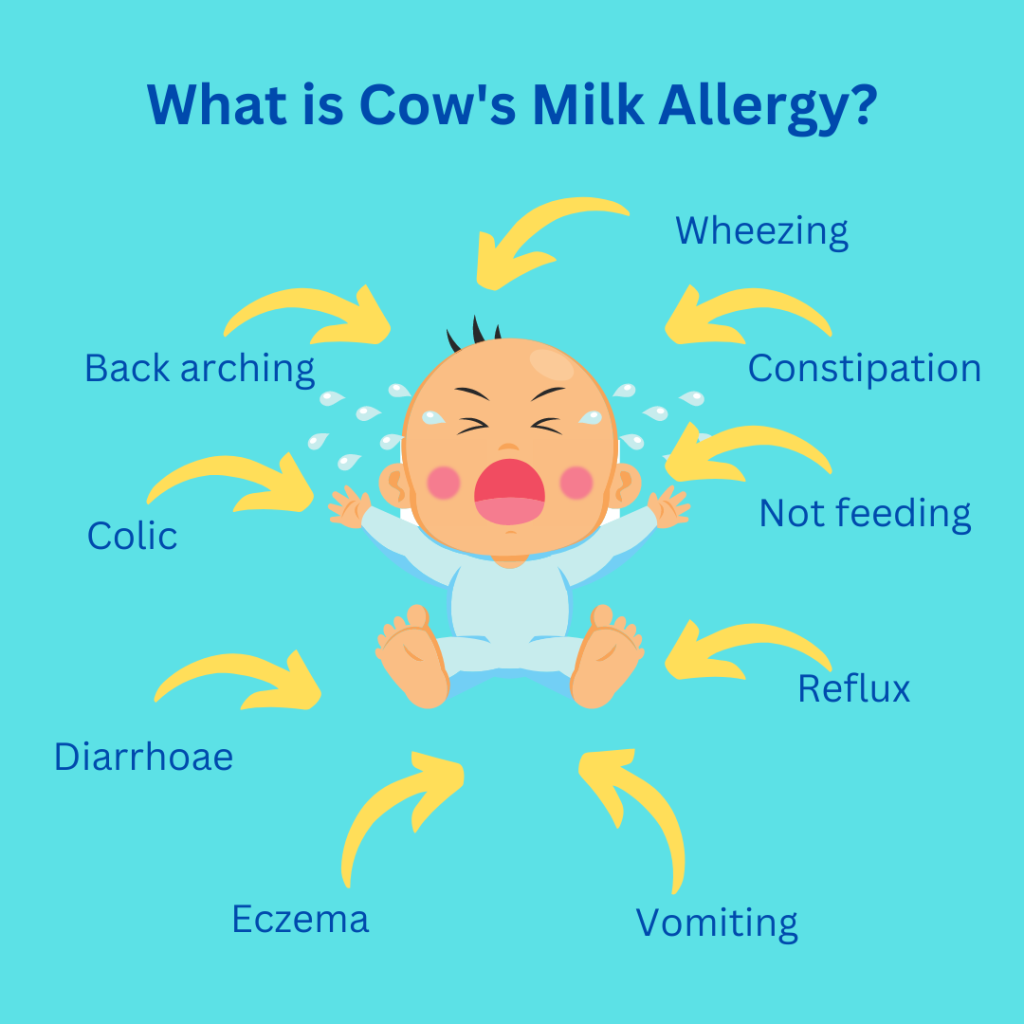
27.How common is cow’s milk protein allergy (CMPA) ?
CMPA usually occurs within the first year of age in up to 2 to 6% of children. Approximately 50% of children have been shown to resolve CMPA within the 1 year of age and 80-90% within 5 years of age .
Source : Caffarelli C, Baldi F, Bendandi B, Calzone L, Marani M, Pasquinelli P; EWGPAG. Cow’s milk protein allergy in children: a practical guide. Ital J Pediatr. 2010 Jan 15;36:5
28. Is hydrolyzed formula milk suitable for patients with AE?
Yes. Extensively or partially hydrolyzed infant formulas are gentle formulas that can reduce the risk of AE among infants with atopy.

29.Are herbal creams safe to use in AE?
Many herbals and/or traditional creams sold over the counter may contain strong steroid that can potentially cause more harm than good. Avoid products that guarantees cure of various skin diseases. Always check with your doctor before applying such creams.
30.If strong steroid creams are harmful, why are there prescribed by doctors to treat AE?
When prescribed professionally and appropriately according to the recommended dose and frequency, steroid creams are the first line therapy that has been proven in many evidence based trials in treating AE effectively.
31.Are steroid jabs recommended regularly?
No. Although such jabs offer near miraculous quick relief, the symptoms will often rebound or recur because the root cause has not been adequately addressed.
32.Why are moisturizers important?
Regular application of moisturizers helps reduce itch, rash and dryness by lubricating, hydrating and preventing water loss from the skin surface.


33.What happens if untreated patients with AE continue to have itch?
Rubbing and scratching due to itch will results in thicker rashes and potential infection which could prolong and render treatment more difficult.

34.Can AE affect the entire body?
Yes. AE can spread to involve > 90% of the skin surface leaving the skin dry, scaly, red.
If AE reaches this stage, other complications arise such as loss of skin hydration, minerals, salts and proteins which could lead to swelling of the body and limbs, heart failure, electrolyte imbalance or infection.

35.Is there any form of therapy that can be done at home to reduce AE symptoms?
Wet wrap therapy. It involves applying moisturizer alone or in combination with a mild steroid cream followed by wrapping the affected areas with a double layer tubular bandage which is wet in the inner layer and dry on the outer layer.
36.Can AE be controlled?
Yes. Seek advice and treatment early from trained and qualified healthcare professionals.
37.Can AE be cured?
New drugs have shown promising results and near complete resolution in cases of severe AE.
The removal of potential allergens, compliance to correct therapy is as imperative as regular follow up with your doctor until AE is well controlled.
Food Allergy
1.What are the common food allergies associated in AE?
Cow’s milk, soy, peanut, egg, shellfish, wheat, fish, tree nuts.

2.What is the likelihood of infants and young children with AE developing food allergy?
About 30% risk.
3.How soon can a patient develop a food allergy?
Within 30-60 minutes hours of ingestion, a patient can develop an antibody (immunoglobulin E) mediated allergic reaction e.g.: itch, wheals, swelling, diarrhoea, vomiting .
A delayed reaction within 24-48 hours is often associated with worsening eczema symptoms.
4.Can food allergies aggravate AE?
Yes, up to 10-30% of infants and children develop worsening AE.
5.If allergy test is positive for specific foods in a patient with AE, should the food be removed from the diet?
Allergy tests can sometimes give false positive results which can lead to unnecessary removal of foods.
Discuss the allergy test results with your doctor for a clear interpretation. A trial of eliminating the specific food from the diet (exclusion diet) may help to identify the culprit food allergen. If exclusion diet was unsuccessful, the reintroduction of the suspected food allergen which will likely worsen the eczema (flare) may be necessary for confirmation.
6.Should the usual culprit foods eg wheat, egg, peanut,cows milk be removed from the patient’s diet?
While these are the common food allergens, it may not be the cause of the allergy per se. Hence unnecessarily eliminating it from the diet will deprive the child’s nutritional needs.
7.If common food allergens were removed from the diet, is it still possible to develop a food allergy in the future?
Yes. If common food allergens that are regularly consumed by a child are removed from the diet, there is still the possibility of the child developing food allergy if the selected food is reintroduced later.
8.Will avoiding common food allergens cure AE?
Avoiding the common food allergens is not likely to cure eczema, but it may help to reduce the severity of symptoms.
Written by:
Consultant Dermatologist
M.D(USM) MRCP(UK) Diploma(AAAM)
Advanced Master in Dermatology(UKM)
KMI Taman Desa Medical Centre